In medical device manufacturing, particularly for high-risk devices like class III implants, maintaining ultra-clean production environments is critical to ensuring product safety and sterility. Managing bioburden – the presence of microorganisms on a product before sterilization – is essential to clean, safe manufacturing practices. Let’s explore the significance of cleanrooms and bioburden management in maintaining the highest standards in medical device production.
The Crucial Role of Medical Manufacturing Cleanrooms

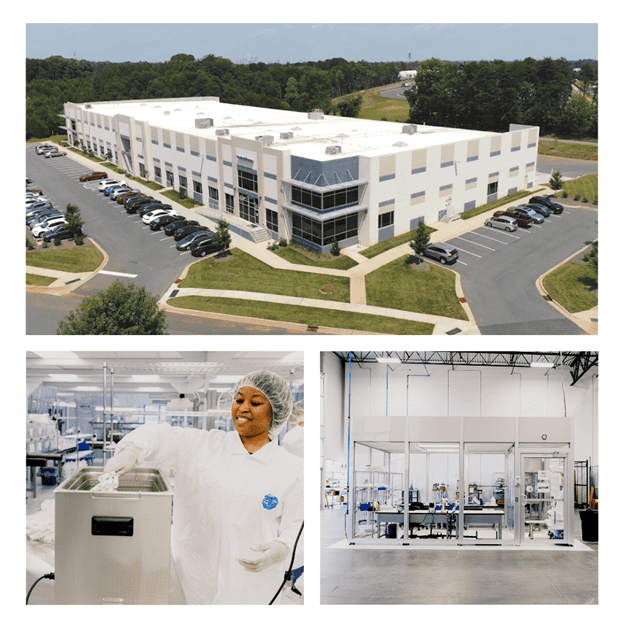
Cleanrooms are specially designed spaces maintaining low levels of environmental pollutants such as dust, airborne microbes, and chemical vapors. They are fundamental in ensuring that medical devices meet health and safety standards, especially for devices intended for use inside the body.
Medical Device Manufacturing Cleanroom Standards and Specifications
The International Organization for Standardization (ISO) provides a classification system for cleanrooms, ranging from ISO 1 (the cleanest) to ISO 9. Class II and III medical devices typically require an ISO 7 or ISO 8 cleanroom. For critical implants or materials that attract debris, an ISO 5 cleanroom or a “cleanroom within a cleanroom” may be necessary.
Factors Influencing Cleanroom Standards
- Device Class: Higher-risk devices necessitate stricter cleanroom conditions.
- Patient Contact and Duration: The level of patient contact dictates the cleanroom standard, especially for long-term implants.
- Sterility Requirement: Absolute sterility demands higher cleanroom standards to prevent microbial and particulate contamination.
- Material Sensitivity: Environmental pollutants’ impact on a device’s materials determines the required level of cleanroom control.
- Complexity of Device: More complex devices require more controlled environments to prevent contamination.
- Regulatory Standards: Compliance with bodies like the FDA and adherence to ISO standards influence the cleanroom class needed.
Special Considerations for Class III Implants

- Advanced air filtration systems, intensive contamination control procedures, and detailed personnel training are essential.
- Validation of cleanroom equipment and processes, constant compliance monitoring, and impeccable record-keeping are crucial.
Understanding Bioburden
Bioburden refers to the viable microorganisms present on a medical device or its packaging. Regular testing is vital to control raw materials, manufacturing processes, and environmental factors.
ISO 11737 and Bioburden Management
Compliance with ISO 11737-1:2018 guides acceptable bioburden levels and necessary actions if exceeded. This standard is integral to continual improvement and safety.
Bioburden Testing Process
Bioburden testing, conducted in accredited facilities, involves sampling production lots. This process is essential for monitoring and controlling various microorganisms like Aerobes, Fungi, and Spores.
Advanced Sterilization and Process Controls
Sterilization methods, such as Ethylene Oxide (EO) Sterilization, are validated for high sterility assurance. Maintaining a controlled environment involves detailed procedures for room maintenance, pest control, and material evaluation.
The role of ultra-clean environments and meticulous bioburden management in the safety of high-risk medical devices is pivotal. For patients receiving these devices, it can means the difference between life and death.
Upholding these standards is a clear indication of a medical device manufacturer’s commitment to safety, quality, and the well-being of patients worldwide. Through rigorous testing, adherence to standards, and advanced sterilization techniques, manufacturers can ensure the highest levels of product safety and sterility.
